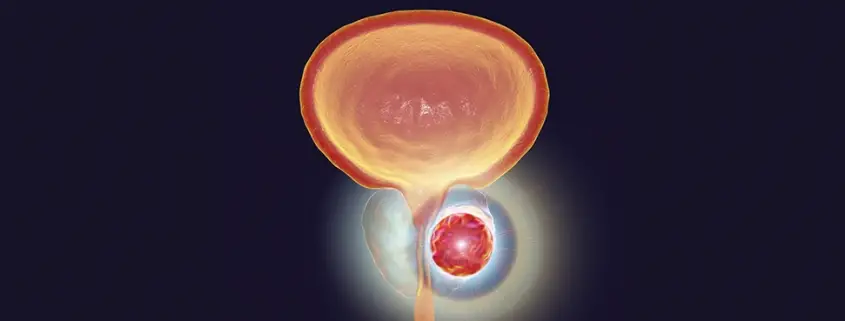
What Is Hepatocellular Carcinoma?
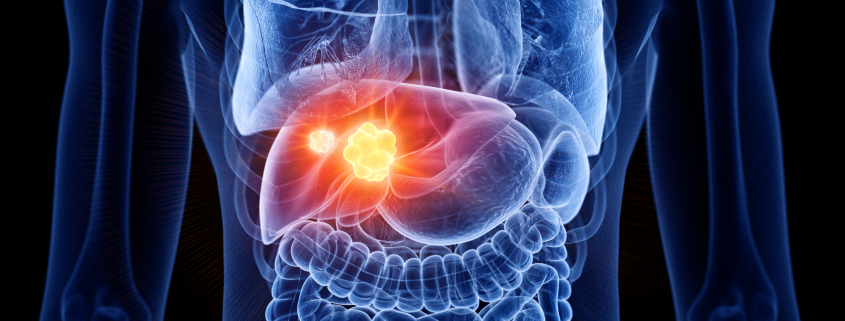
Hepatocellular Carcinoma (HCC) is the most prevalent type of primary liver cancer. Primary liver cancer is cancer that starts in the liver, whereas secondary liver cancer is cancer that has metastasised or spread from another part of the body to the liver.
Roughly 90% of all cases of liver cancer appear in this form. It is the 3rd leading cause of all cancer deaths worldwide and is particularly common in developing countries. It affects roughly 2.5 people for every 100,000 people in the population. It is more than two times more common in men than in women and is more prevalent in Eastern and Southern Asia, Middle and Western Africa. The median survival rate is approximately 6 to 20 months from the time of diagnosis.
Hepatocellular Carcinoma tends to have two distinct growth patterns; a single tumour that grows to a significant size before spreading or as many small cancer nodules throughout the liver.
What Causes Hepatocellular Carcinoma?
The exact cause of Hepatocellular Carcinoma is not known, but it is found most commonly in people with underlying liver conditions such as hepatitis B or C, hemochromatosis, biliary stent disorder or fatty liver disease. These conditions end up causing cirrhosis, which in simple terms is ‘liver scarring’.
As the liver gets damaged by these conditions, scar tissue forms on the liver as it attempts to repair itself. Damage caused by cirrhosis is permanent, so the liver is forced to make new cells to improve overall liver function.
There is a risk of these new cells mutating and becoming cancer cells. The more cells grown in this way, the higher the chances that a mutation can occur.
What Are the Symptoms of Hepatocellular Carcinoma?
Hepatocellular Carcinoma will show up the same as many other conditions that indicate poor liver health, such as:
- Abdominal pain,
- Ascites (abnormal buildup of fluid in the abdomen)
- Bloating
- Bone pain
- Nausea
- Vomiting
- A lump or mass under the ribs
- Loss of appetite
- Sudden weight loss
- Shortness of breath
- Itching
- Jaundice
How Is Hepatocellular Carcinoma Diagnosed?
There are three main ways in which Hepatocellular Carcinoma is diagnosed; Lab tests, Imaging Tests, and Biopsies.
Lab Tests
- Alpha Fetoprotein Blood (AFP) Test
AFP is a protein that is found in healthy adults at very low levels.
High AFP levels in adults indicate the possibility of liver cancer and is the most used tumour marker test for Hepatocellular Carcinoma. The test is typically carried out with several others.
- Liver Function Tests (LFTs)
As liver cancer is most often the result of an already debilitated liver, LFTs serve as a good indicator of liver health. They can help understand which parts of the liver have been damaged and to what extent.
Typically, LFTs test for alanine transaminase (ALT), aspartate transaminase (AST), alkaline phosphatase (ALP), gamma-glutamyl transferase (GGT), serum bilirubin, prothrombin time (PT), the international normalised ratio (INR) and albumin.
- Des-Gamma-Carboxy Prothrombin (DCP) Test
The DCP test is another cancer marker lab test much like AFP. It is also known as protein induced by vitamin K absence-II (PIV-KAII).
This test is used in conjunction with AFP tests as it tends to show elevated levels in individuals who have Hepatocellular Carcinoma but who do not show elevated AFP levels.
Imaging Tests
- Ultrasound
The ultrasound is usually the very first test used to check for tumours in the liver. It makes use of sound waves to create images on a computer. The tumours typically show up as dark grey (hypoechoic) masses.
- Computed Tomography (CT) Scan
Specialised X-ray equipment is used to conduct a CT scan to produce cross-sectional images of the liver. Specific information about the size, shape and location of possible tumours can be evaluated.
Liver lesions typically show up as masses or areas of abnormal enhancement on multiphasic CT imaging, which in conjunction with blood markers and clinical history, can help the clinician come to a definitive diagnosis.
- Magnetic Resonance Imaging (MRI) Scan
MRI Scans are typically ordered if the CT scan was unable to confirm the diagnosis. MRIs also produce cross-sectional imagery but make use of radio waves instead of X-rays.
MRI scans can be more accurate and give better imagery in certain circumstances but usually are more costly. Identification requires a skilled assessment of the images.
- Positron Emission Tomography (PET) Imaging
Positron Emission Tomography / Computed Tomography (PET/CT) imaging is a form of hybrid molecular imaging that uses radiotracers to detect and image molecular changes in the body.
For liver tumours, the more commonly used radiotracers are Fluorodeoxyglucose and Acetate. These tracers are used in metabolic pathways found in hepatocellular carcinomas, and by means of such molecular imaging, we can pinpoint and detect active tumours.
Biopsy
A biopsy is the most definitive diagnostic test that can be carried out for Hepatocellular Carcinoma.
It is the process of the removal of a piece of liver tissue for laboratory testing. The removed tissue cells are studied under a microscope, whereby cell mutation can be confirmed as cancerous.
What Are the Treatment Options Available for Hepatocellular Carcinoma?
Several different treatment options are available for Hepatocellular Carcinoma, and it is not a one-size-fits-all approach. Depending on the individual’s stage, severity, and overall health, different combinations of treatments may be recommended.
Hepatocellular Carcinoma can be somewhat challenging to treat because of how the disease presents itself, developing in a background of cirrhosis, making it difficult to target exclusively.
1) Radiation
Radiation therapy is the use of high energy beams of protons. The beams are targeted and focused at the cancer cells to kill them while carefully avoiding damage to healthy liver cells.
Radiation therapy is typically recommended when other treatment options are unsuitable. Radiation therapy also has been shown to play an essential role in downstaging patients who are not eligible for transplant due to the extent of their cancer, possibly improving their condition to make transplant a viable option for them.
Some of the more common side effects of radiation therapy include:
- Diarrhoea
- Fatigue
- Loss of appetite
- Nausea and vomiting
- Radiation-Induced Liver Disease
- Redness to blistering and peeling close to radiated location
2) Chemotherapy
Chemotherapy is the use of drugs that are taken orally or intravenously to kill cancer cells. The drugs can be administered systemically (when cancer has spread) or regionally (more targeted).
The drugs can also be administered directly into the hepatic artery through a method called Hepatic Artery Infusion so that a higher dose of drugs can be issued. This form of receiving the drugs is done under general anaesthesia and requires an infusion pump.
Compared to radiation, it is considered a non-targeted form of treatment as the drugs affect more than just the cancer site and may result in many unwanted side effects.
The severity and type of side effects depend on the individual and the type and dosage of the drugs prescribed. The most common chemotherapy drugs used for treating Hepatocellular Carcinoma are:
- Gemcitabine (Gemzar)
- Oxaliplatin (Eloxatin)
- Cisplatin (Platinol)
- Doxorubicin (Adriamycin)
- 5-fluorouracil (Adrucil)
- Capecitabine (Xeloda)
- Mitoxantrone (Novantrone)
These drugs are often used two or three at a time in combination with each other to achieve the best results.
Some of the more common side effects of chemotherapy include:
- Diarrhoea
- Easy bruising or bleeding
- Fatigue
- Hair loss
- Increased chance of infections
- Loss of appetite
- Mouth sores
- Nausea and vomiting
3) Targeted Therapy
Whereas chemotherapy is non-targeted, other drugs can be used for treatment that is targeted. These drugs target the liver specifically instead of being dispersed throughout the entire body and are known as Targeted Therapy. There are two main types of targeted therapies; small molecule medicines and monoclonal antibodies.
Small molecule medicines enter into cancer cells and destroy them, while monoclonal antibodies work by attacking targets outside the cell to destroy them.
Small molecule medicines can be identified via their generic names ending with -ib, while monoclonal antibodies have their generic names ending with -mab.
These drugs work in a variety of ways and have many different mechanisms of action. Targeted therapy works in one of the following ways:
- Stopping the creation of new blood vessels that feed the cancer cell
- Activating the immune system to attack the cancer cell
- Altering proteins within the cancer cell
- Shutting down signals that inform the cancer cell to grow or divide
- Transporting toxins into the cancer cell
Popular small molecule medicines for early treatment of Hepatocellular Carcinoma are Sorafenib (Nexavar) and Lenvatinib (Lenvima), while Regorafenib (Stivarga) and Cabozantinib (Cabometyx) are used in more advanced stage treatment.
A popular monoclonal antibody for early treatment of Hepatocellular Carcinoma is Bevacizumab (Avastin), while Ramucirumab (Cyramza) is used in more advanced stage treatment.
Some of the more common side effects from targeted therapy include:
- Bleeding
- Diarrhoea
- Headaches
- High blood pressure
- Loss of appetite
- Low white blood cell counts
- Mouth sores
- Tiredness
4) Immunotherapy
As the name suggests, immunotherapy is a treatment that uses the body to activate the immune system to combat cancer.
Cancer cells tend to mask themselves by turning on proteins that are known as Immune Checkpoint Proteins. When cancer cells use these, they tell the body’s immune system to leave them alone.
Most immunotherapy drugs work by blocking the binding of the cancer cells to these Immune Checkpoint Proteins and are called Immune Checkpoint Inhibitors.
These drugs can be classified as either PD-1 and PD-L1 inhibitors or CTLA-4 inhibitors. Commonly used immune checkpoint inhibitors for Hepatocellular Carcinoma are Atezolizumab (Tecentriq) and Ipilimumab (Yervoy).
Some monoclonal antibody targeted therapies are also forms of immunotherapy. One example is Rituximab (Rituxan), which marks cancer cells so that the immune system learns to better identify them and destroy them.
Some of the more common side effects from immunotherapy include:
- Constipation or diarrhoea
- Cough
- Itching
- Feeling tired or weak
- Fever
- Loss of appetite
- Muscle or joint pain
- Nausea
- Skin rash
5) Surgery
Surgery is usually the best option to cure liver cancer as it is the total removal of the tumour and all cancer cells. The procedure is called a partial hepatectomy, which removes part of the diseased liver.
The downside here is that only people with a relatively healthy liver with a single tumour and where the cancer has not metastasised into the blood vessels can have this operation.
The feasibility of the procedure is evaluated via imaging tests. Still, it is also possible that during surgery, the cancer might be found to have grown too large or spread too much, resulting in the surgery being aborted.
Though it may be the best option, it does come with a lot of risks and side effects:
- Bleeding during and after surgery
- Blood clots
- Complications from anaesthesia
- Infection
- Pneumonia
6) Liver Transplant
When removal of part of the liver is not an option, and other forms of treatment have proved unsuccessful, a total replacement of the liver via a liver transplant is the best way for a chance at being cured.
The vast majority of liver transplants come from people who die in accidents or from a donor in the family. The liver has unique regenerative properties, and a portion of it can be donated from a living donor to someone in need of a transplant safely.
Just like with partial hepatectomy, there are significant risks involved in a liver transplant:
- Bleeding during and after surgery
- Blood Clots
- Complications from anaesthesia
- Infection
- Rejection of the new liver
7) Theranostics
Theranostics is the act of using a combination of radiation-based drugs to identify and then kill cancer cells. One drug is used for the identification, and another is used for the treatment – providing a 2 in 1 solution of Therapy plus Diagnostics or Theranostics.
For treatment of Hepatocellular Carcinoma, in the diagnosis stage, a test study using Technetium 99m Macroaggregated Albumin (MAA) is done to determine the uptake of such particles. These are injected into the liver via the hepatic artery, and following the injection, a scan is done to determine the distribution of particles in the cancer and normal tissue.
By means of such testing, we are then able to determine an appropriate radiation dose to treat the cancer and yet limit the amount of radiation to normal tissue.
In the therapy stage, the therapy agent used is Yttrium-90 microspheres. The technique involves delivering Yttrium-90 infused microspheres via the hepatic artery, similar to the initial testing phase.
The tumour then receives a highly concentrated dose of radiation while the surrounding healthy liver cells receive a much-reduced amount.
Some of the potential side effects from Yttrium-90 SIRT include:
- Gastritis/Duodenitis
- Lethargy
- Mild to moderate fever
- Nausea
- Radiation-Induced Liver Disease
Who Will Benefit from Treatment with Yttrium-90 Selective Internal Radiation Therapy (SIRT)?
The people who benefit most from Yttrium-90 SIRT are those with inoperable tumours that cannot be removed during surgery or where other treatment options have not proved to be beneficial.
What Are Some Questions I Should Be Asking My Doctor When Considering Treatment Options for Hepatocellular Carcinoma?
- Has the cancer spread beyond the Liver?
- What stage of cancer do I have?
- What treatment options would you recommend?
- What are my chances of survival based on what you can see?
- How much experience have you had treating this kind of cancer?
- Should I consider getting a second opinion?
- Should I consider taking part in a clinical trial for new treatments?